Coronary Angiogram
The gold standard procedure for examining how well blood is flow through the arteries of the heart, a coronary angiogram utilises a dye (contrast) introduced into the blood vessels at the same time as sequences of x-ray images (fluoroscopy) are seen and recorded from several different angles (projections).
Doing this enables the Cardiology Consultant to observe in real time the exact route blood is taking to reach the heart muscle (myocardium).
Access to an artery is required and those most commonly used are in the wrist (radial) or the top of the leg (femoral), firstly local anaesthetic is injected under the skin of the area being used, this does sting briefly however it works very well to numb the area for the remaining procedure. Once numb a small tube (sheath) is inserted into the artery which enables smaller tubes (catheters) to be used to reach the heart to introduce dye. It is safer to perform the procedure whilst you are awake, however sedation is available if required.
Coronary Angioplasty
Using a very similar process as an angiogram, the angioplasty progresses further and involves opening any narrowings or restrictions sufficient enough to significantly reduce the flow of blood to the heart muscle.
To do this a tiny balloon is advanced through a catheter not unlike that required for the angiogram, and on to the narrowing which could be a soft or hard lesion. The balloon is then inflated at a pressure high enough to push the lesion flat against the walls of the artery, this may be performed several times in order to produce a satisfactory result.
To keep the area open long term a metal tubular mesh is then introduced over another balloon which is inflated pressing the mesh against the walls of the affected artery. It’s not unusual to feel chest discomfort while inflations are taking place, this is often a good sign that effective treatment is taking place.
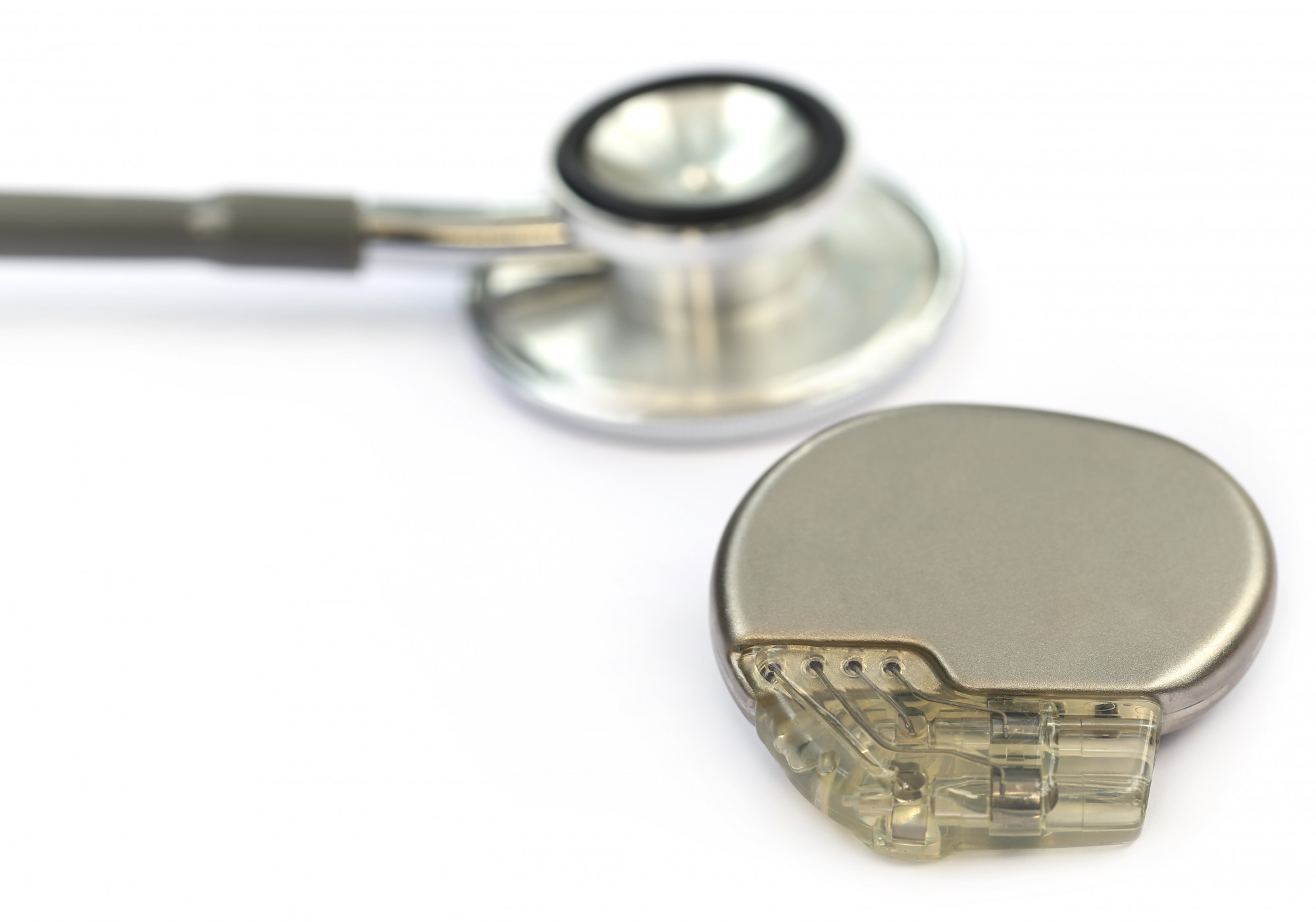
Pacemaker Implant
A pacemaker is used to address problems arising from the heart's own electrical conduction system, which mainly consists of a natural pacemaker and network of “wiring” and as with the wiring in our own homes, this can degrade over time or have problems associated with damage or injury.
If this causes the heart's rhythm to become slow enough to cause symptoms such as dizziness, loss of consciousness or simply be an incidental finding indicating a dangerously slow rhythm, then a pacemaker is an ideal way to overcome that “wiring” fault.
As with many procedures it is safer to perform awake although sedation is available, the operator will inject local anaesthetic under the skin usually in the upper left or right chest area. Stinging initially the local anaesthetic will numb the area and reduce any discomfort for the remaining procedure. A small incision is then made and a vein found of the ideal size to accommodate very thin and flexible pacing wires. Veins travel naturally back to the heart and so are ideal to use for introducing pacing wires to the chambers on the right side of the heart.
Pacemakers used to address slow heart rhythms will require either one or two pacing wires depending on the nature the conduction problem. Pacing wires are normally introduced using X-Ray and once these wires are positioned in the heart chambers they will be tested, which includes pacing the heart in order to ensure the location is ideal. If not ideal the wires can be re-positioned and the tests repeated until optimal test results are obtained. It is not unusual to feel an irregular, skipped, or rapid heart-beat while the wires are positioned and tests are performed.
The stability of pacing wires is maintained in the heart with either small wings (tines) or a tiny screw at the tip of the wires. They are also secured with stitches under the skin after the point they exit the vein. Once secure the pacing wires are connected to the pacemaker with is the placed into a small pocket under the skin. Finally the skin closed with dissolvable stitches and glue.
CRT-P Implant
Cardiac Resynchronisation Therapy Pacemaker Implant, also called a Biventricular Pacemaker: these are implanted for hearts which have become less effective as a pump.
Designed to pace all the time and synchronise the left and right side of the heart an extra pacing wire is required. The procedure is very similar to a pacemaker implant however a pacing wire is also positioned on the left side of the heart, this can take a little longer than a standard pacemaker procedure.
Implantable Cardioverter Defibrillator (ICD) Implant
A modern ICD can be described as a pacemaker with a larger battery, which enables it to shock the heart if someone is at risk of going into a very fast and dangerous rhythm pattern.
Although very similar to a Pacemaker Procedure it is normally performed under sedation and general anaesthesia.
CRT-D Implant
Cardiac Resynchronisation Therapy Defibrillator Implant, also called a biventricular ICD: this is for people whose heart is less effective as a pump and at risk of dangerously fast rhythm patterns.
The procedure is very similar to an ICD implant however just like a CRT-P, an extra wire is required on the left side of the heart which will take a little longer than a pacemaker and ICD procedure.
Insertable Cardiac Monitor Procedure
Also called a loop recorder, this is a very small device, which continuously records the electrocardiogram (ECG) or heart rhythm.
Monitoring can continue for at least three years during which the device can recognize normal heart rhythms and abnormal rhythms in twenty second snapshots (twice as long as a standard ECG). The device also comes with a small widget, which can be triggered by the patient to instruct the monitor to a store a longer recording if the worst symptoms are experienced.
The procedure itself may only take a few minutes. Starting with some local anaesthetic under the skin on the left side of the chest, which may sting. A small puncture is then made and the monitor inserted.